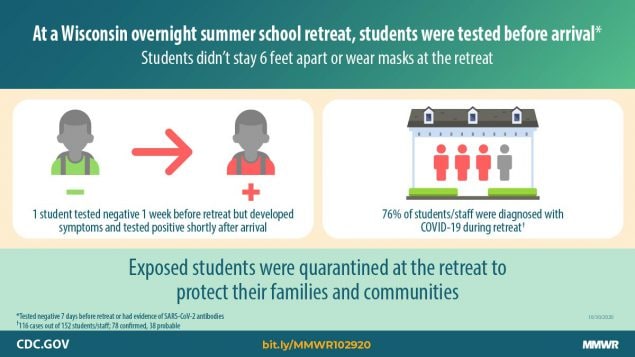
A group of youngsters caught the Covid-19 virus at a Wisconsin church retreat last summer. One kid tested negative before arriving but managed to catch it from a relative. The kids stayed in dorms together and didn't practice social distancing. However, the CDC said most of the infected only had mild symptoms. The CDC reports:
During July 2–August 11, 2020, an outbreak of coronavirus disease 2019 (COVID-19) occurred at a boys’ overnight summer school retreat in Wisconsin. The retreat included 152 high school-aged boys, counselors, and staff members from 21 states and territories and two foreign countries. All attendees were required to provide documentation of either a positive serologic test result* within the past 3 months or a negative reverse transcription–polymerase chain reaction (RT-PCR) tests result for SARS-CoV-2 (the virus that causes COVID-19) ≤7 days before travel, to self-quarantine within their households for 7 days before travel, and to wear masks during travel.
On July 15, the Wisconsin Department of Health Services (WDHS) began an investigation after being notified that two students at the retreat had received positive SARS-CoV-2 RT-PCR test results. WDHS offered RT-PCR testing to attendees on July 28 and serologic testing on August 5 and 6. Seventy-eight (51%) attendees received positive RT-PCR results (confirmed cases), and 38 (25%) met clinical criteria for COVID-19 without a positive RT-PCR result (probable cases). By the end of the retreat, 118 (78%) persons had received a positive serologic test result. Among 24 attendees with a documented positive serologic test result before the retreat, all received negative RT-PCR results. After RT-PCR testing on July 28, WDHS recommended that remaining susceptible persons (asymptomatic and with negative RT-PCR test results) quarantine from other students and staff members at the retreat. Recommended end dates for isolation or quarantine were based on established guidance (1,2) and determined in coordination with CDC. All attendees were cleared for interstate and commercial air travel to return home on August 11.
This outbreak investigation documented rapid spread of SARS-CoV-2, likely from a single student, among adolescents and young adults in a congregate setting. Mitigation plans that include prearrival quarantine and testing, cohorting, symptom monitoring, early identification and isolation of cases, mask use, enhanced hygiene and disinfection practices, and maximal outdoor programming are necessary to prevent COVID-19 outbreaks in these settings (3,4).
Investigation and Findings
Students and staff members (two teachers, one principal, and one emergency medical technician) traveled from 21 states and territories and two foreign countries to attend a faith-based educational retreat for boys in grades 9–11. In an effort to prevent introduction of COVID-19, all attendees were required to provide documentation of either a positive serologic test result within the past 3 months or a negative SARS-CoV-2 RT-PCR result ≤7 days before travel, to self-quarantine within their households for 7 days before travel, and to wear masks during travel. At the retreat, students and counselors were not required to wear masks or social distance, and students mixed freely. Classes were held in outdoor pavilions with approximately 20 students per class seated <6 feet (<2 m) apart at tables. Teachers wore masks during class and were socially distanced from students at all times. The 127 students resided in dormitories (four to six per room) and yurts (eight per room), organized by grade. Beds in dormitory rooms and yurts were tightly spaced with three to four sets of bunks each, shared bathrooms, and shared common areas. Counselors (21; aged 17–24 years) roomed together in dormitories and yurts, and the four staff members resided in four separate housing units.
On July 2, students traveled by air and ground to a regional hub, met with counselors and staff members, and boarded three buses to the retreat (Figure). On July 3, a ninth-grade student (the index patient) who had received a negative RT-PCR result <1 week earlier experienced sore throat, cough, and chills, and received a positive RT-PCR result on July 5. This student later learned that a family member received a positive RT-PCR result approximately 1 week after his departure. At the retreat, he was isolated in a private room, and 11 of his close contacts (including four roommates) were quarantined together in a separate dormitory. The 11 contacts received negative rapid SARS-CoV-2 antigen results and were released from quarantine on July 7, but neither the tests that were conducted nor the results could be verified by public health. During July 4–7, six of 11 close contacts of the index patient and 18 additional students with unknown exposure histories reported new onset of mild symptoms. These students were given masks, but contact tracing was not done and the students were not isolated. On July 13, a second student (one of the 11 initial close contacts of the index patient) received a positive RT-PCR test result at a local clinic. On July 15, WDHS was notified and initiated an outbreak investigation. WDHS instructed retreat organizers in mitigation measures such as symptom monitoring, isolation of symptomatic attendees, and quarantine of contacts, but the capacity for such measures was exceeded by the large volume of symptomatic attendees.
On July 28, WDHS coordinated RT-PCR testing for 148 (97%) of 152 retreat attendees. At the time of specimen collection, no new illnesses had occurred since July 20. During August 5–6, WDHS returned to collect a serum sample for serologic† testing from 148 (97%) attendees; 145 (95%) attendees received both tests. Positive RT-PCR isolates with sufficient cycle threshold values (six of 82; 7%) were analyzed with whole genome sequencing.§
A confirmed COVID-19 case was defined as receipt of a positive SARS-CoV-2 RT-PCR test result after July 2 in a retreat attendee. A probable case was an illness meeting clinical criteria for COVID-19 (5) with symptom onset during the retreat in an attendee with no prior serologic results who was either not tested by RT-PCR or received a negative RT-PCR result on a sample obtained ≥10 days after symptom onset (to account for attendees who might have cleared the virus by the time of RT-PCR specimen collection). Serologic results were not used for case classification. All analyses were performed using Stata (version 14.2; StataCorp). Fisher’s exact test was used for attack rate comparisons; p-values <0.05 were considered statistically significant. This investigation was reviewed by WDHS for human subjects’ protection and determined to be nonresearch.
Among 152 attendees, 116 (76%) were classified as having confirmed (78; 51%) or probable (38; 25%) COVID-19. Thirty-four (89%) attendees with probable COVID-19 received negative RT-PCR test results on specimens obtained 11–22 days (median = 16 days) after symptom onset. Among the 148 attendees who underwent serologic testing at the end of the retreat (four attendees refused testing), 118 (80%) received positive results. This included 30 (81%) of 37 attendees with probable COVID-19 (one missing), 65 (86%) of 76 with confirmed COVID-19 (two missing), 16 (70%) of 23 attendees with positive serology before the retreat (one missing), and seven (58%) of 12 attendees without a COVID-19 diagnosis or prior serologic result (Table 1). Whole genome sequences for RT-PCR–positive isolates from six attendees differed by 0–1 single nucleotide polymorphisms, suggesting a common source for these six attendees.
At least one confirmed case occurred in every dormitory room and yurt (Supplementary Figure, https://stacks.cdc.gov/view/cdc/95625). Attack rates did not differ significantly among counselors and students, dormitories and yurts, or grade levels (Table 2). All four staff members received negative RT-PCR test results; one staff member (an emergency medical technician) was classified as having a probable case. To comply with the retreat’s attendance requirements, 24 (16%) attendees provided documentation of a positive serology results before the retreat. All 24 received negative RT-PCR results. Six (25%) experienced mild symptoms at the retreat but were not classified as having confirmed or probable COVID-19. Excluding the 24 attendees with previous positive serologic results, the COVID-19 attack rate on the remaining susceptible population was 91% (116 of 128). One (1.2%) of 78 persons with a positive SARS-CoV-2 RT-PCR test result was asymptomatic. All illnesses were mild to moderate, and no hospitalizations or deaths occurred.
Public Health Response
When WDHS initiated the investigation on July 15, retreat staff members reported that the majority of students had recovered from mild illnesses. After RT-PCR testing on July 28, WDHS recommended that remaining 36 susceptible persons (24%; asymptomatic and with negative RT-PCR test results) quarantine from other students and staff members at the retreat. Recommended end dates for isolation or quarantine were based on established guidance (1,2) and determined in coordination with CDC’s Division of Global Migration and Quarantine. Outdoor coursework and recreational programming were able to continue for the duration of the retreat, and all attendees were cleared for interstate and commercial air travel to return home on August 11.
Discussion
Extensive and rapid transmission of SARS-CoV-2 occurred at an overnight retreat where adolescents and young adults aged 14–24 years had prolonged contact and shared sleeping quarters. A single student, who received a negative SARS-CoV-2 RT-PCR test result <1 week before the retreat and experienced symptoms 1 day after arriving, was the likely source of introduction, resulting in infection of 76% of attendees. Similar rapid spread has been described among younger children in overnight camps (6,7) and adults in congregate settings (8,9).
Nonpharmaceutical interventions have been effective in preventing SARS-CoV-2 transmission at overnight camps (3). Effective measures include prearrival quarantine and testing, cohorting, symptom monitoring, physical distancing, mask use, enhanced hygiene measures, enhanced cleaning and disinfection, outdoor activities and programming, and early identification of infections and isolation. At this retreat, organizers required documentation of a negative prearrival RT-PCR result, 7-day prearrival quarantine, and outdoor programming, but did not implement other recommended nonpharmaceutical interventions. The capacity of retreat organizers to contain transmission through isolation and quarantine early in the outbreak was exceeded given the large number of persons exposed and experiencing symptoms. A robust COVID-19 mitigation plan that included a full 14-day prearrival quarantine might have prevented introduction of SARS-CoV-2 in this setting. As well, cohorting of attendees for 14 days after arrival might have permitted early containment of the outbreak. Finally, earlier engagement with public health authorities to discuss recommended mitigation strategies (4) might also have aided prevention and control efforts.
An important feature of this outbreak was that 24 attendees had documented evidence of antibodies to SARS-CoV-2 before arrival. None of these persons received a positive SARS-CoV-2 RT-PCR test result at the retreat. Evidence to date is insufficient to determine whether the presence of detectable antibodies indicates protective immunity¶ or how long such immunity might persist. The absence of RT-PCR–confirmed infections among persons with previous positive serology results suggests that some protective effect was present, given the high attack rate observed at the retreat.
The proportion of SARS-CoV-2 infections that were asymptomatic (1%) in this population was low, compared with those described in other published reports (10). Retreat staff members kept detailed symptom logs for students, which likely facilitated improved ascertainment of mild or delayed COVID-19 symptoms, compared with other settings and might explain the low rate of asymptomatic infection observed. In addition, some mild symptoms experienced by attendees possibly were not related to infection (e.g., allergies or travel fatigue) or were caused by another viral illnesses, which would have led to overestimation of the number of probable cases.
The findings in this report are subject to at least four limitations. First, RT-PCR testing was conducted after the outbreak (no new illnesses in the 8 days before testing), likely leading to underestimation of the number of confirmed cases. Second, baseline serology results were not available for all retreat attendees. Some positive results in follow-up serologic testing might have been caused by past undocumented infections rather than SARS-CoV-2 infection at the retreat. Third, dates of prior illnesses among attendees with previous positive serologic results were not known, and the duration of possible acquired immunity against SARS-CoV-2 infection could not be assessed. Fourth, the definition for probable COVID-19 used in this investigation was adapted from the Council of State and Territorial Epidemiologists interim COVID-19 case definition (5) to account for the delay in RT-PCR testing and availability of prior serologic results for some attendees; results may not be comparable with other outbreak investigations.
SARS-CoV-2 can spread rapidly among adolescents and young adults in a congregate setting with inadequate COVID-19 mitigation measures. These findings provide preliminary evidence that detectable antibodies might provide protection against new SARS-CoV-2 infections for an unknown duration. A robust COVID-19 mitigation plan developed in collaboration with public health authorities is important for preventing and containing similar outbreaks at overnight camps and residential schools. Avoidance of travel for attendees who were in isolation or quarantine likely prevented transmission to communities and family members during this outbreak and could be considered in COVID-19 mitigation plans for other congregate settings. To prevent introduction of COVID-19, mitigation plans should also include prearrival quarantine, prearrival and postarrival testing and symptom screening, the ability to isolate and quarantine, cohorting, physical distancing, mask use, enhanced hygiene and disinfection, and maximal outdoor programming (3). CDC report.

























19 comments:
We should test less, that will fix this pandemic.
-Morons
Hmmmh, a bunch of kids got a cold, go figure.
Wonder if 78% of the kids had parents or grandparents or immune suppressed relatives?
@10:12 they actually got COVID-19, not a cold. You don’t read so good do you?
@10:12 - and world war 2 was just a tickle fight. No more than a verbal disagreement really.
I thought kids couldn't spread the virus. So much for that theory. I guess it is good mitigation that keeps the spread under control at schools rather than an inherent protection in children. Keep that in mind for the upcoming holidays, you may want to rethink that Thanksgiving or Christmas gathering. All it takes is one person to infect dozens.
Just wail til after the election to see just how bad it is really spreading.
No one said kids don't spread it. They aren't superspreaders and when they get it, the cases tend to be light. That means the viral load is probably less in kids.
This was not a Vacation Bible School where the kids are sent home every day and protocols are followed. The kids were living together round the clock. 6-8 to a room. No distancing and no masks (yeah I know the debate over that one). Not how I would have done it.
The bright side is the report says the symptoms were mild. If true, that is encouraging news among kids.
There is no story here.
Of course they had mild symptoms. They haven't yet had several decades of oxidation to their bodies combined with all the carcinogens we love to ingest.
Kids are going to be fine. Healthy adults will be okay as well. Megadose your vitamins and dont be a drunken fatass. Morbid obesity will kill you.
Why is this news? Kids get sick all the time. Ever had a kid in daycare?
Love the way most feel this is actually a end of time scenario. Using numbers supplied by WHO, CDC, ECDC and NHC we have 45,360,632 (World cases confirmed positive which doesn't mean shit as it's not qualified) is 0.648% of the population. With 1,185,053 dead (supposedly related to, but not confirmed as a direct reason/cause of death) is 0.016% of the world. World infection and death rate is using 7,000,000, people.
US infected number is 1,185053 and using US population of lets just say 350,000,000 that translates to 2.57% of US population. Not exactly on the precipice. Our so called Covid related deaths of 229,293 relates to 0.065% of our US population. Neither is even remotely close to plagues and disease like the black Death, Swine Flu, or the Yellow Fever of 1793. The yellow fever epidemic in Philadelphia, 5,000 or more people were listed in the official register of deaths between August 1 and November 9. The vast majority of them died of yellow fever, making the epidemic in the city of 50,000 people one of the most severe in United States history.
With a very high survival rate of over 95+% ,yeah, it's a fucking cold.
@10:46 Covid is a type of coronavirus, and coronaviruses the second most likely cause of the common cold after rhinovirus. "All illnesses were mild to moderate, and no hospitalizations or deaths occurred." This study is a description of a virus that caused cold symptoms spreading through a camp.
You're right on Kingfish, the great majority of the spread has been documented to be in households with extended close contact.
My wife and I had it. She had a very mild fever, but I never had one. I was sore one day, but I'm very active and it was like the day after a long run or hard workout. Neither of us lost taste or smell. We were both fatigued for a day each and we both thought we were just getting our annual sinus infections.
A bunch of people are out there unknowingly spreading it, but a bunch of people are also out there knowingly spreading it because they can't or won't be quarantined. COVID is real but it's not a big deal if you're reasonably healthy. (Yeah, that's not most of Mississippi. I get it.)
Bottom line: Protect the vulnerable, but the rest of us should be able to get on with our lives.
Everything is and will be Covid. As St Fauci says, "Theres Gold in them thar hills".
"My wife and I had it. She had a very mild fever, but I never had one. I was sore one day, but I'm very active and it was like the day after a long run or hard workout. Neither of us lost taste or smell. We were both fatigued for a day each and we both thought we were just getting our annual sinus infections. "
Dude . . . you just described a hangover.
How much did you and the wife drink the night before.
And 100% recovered.
If they gave IQ tests like they are testing for Covid, we'd see an rising epidemic of morons.
All of you people who think you're immune to getting sick and dying, please stay away from me. I don't want to catch your cold, your flu, and I sure don't want to catch your COVID. It doesn't matter to me if it's mild or not, I don't want it and I don't want my child getting it.
Post a Comment